A number of amazing startups have been popping up of late to employ modern technology in the hopes of improving healthcare and education. This is important not only because these are two industries that touch each and every one of us, but because they are both equally consumed by legacy infrastructure and archaic standards. Yet, while startups continue to enter the space — something we should continue to celebrate — many are still shying away from some of the most challenging technical problems that stand to make a bigger impact than yet another sexy consumer mobile app.
Granted, this shouldn't be surprising, given that both industries suffer from some seriously intractable problems, mostly courtesy of long-entrenched legacy infrastructure. Modernizing the infrastructures themselves, along with the way health companies integrate and exchange data is a difficult task — but it's also an important one.
Eligible, a San Francisco-based startup and member of Y Combinator's most recent batch, has decided to bite the bullet and meet this challenge head on. Big data stands to have a transformative effect on healthcare (and education and really every industry), but the key is putting that data in a language that is smart, universal and dynamic.
To do that, Eligible set out to build a modern, standardized set of protocols to make healthcare data and information more accessible, particularly healthcare eligibility. A member of the same Y Combinator class as Clever, Eligible is applying the same philosophy to healthcare data. In other words, just as as Clever (and LearnSprout) have created a modern set of REST APIs to unlock student data from the lumbering, closed datasets of Student Information Systems, Eligible is doing the same for healthcare eligibility.
The goal is to pull down the barriers that restrict the interoperability of disparate (yet critical) data sets, making them easier to manage and integrate. Of course, "healthcare eligibility" is a side of the healthcare infrastructure that the average person doesn't see much of, and thus it may seem a bit boring or obscure (because it is), but it's also an essential part of the process of receiving and managing care and is part of making the whole thing tick.
For example: Every time you go to the doctor's office, seek treatment or go in for surgery, hospitals and doctors query insurance companies to see what kind of coverage you have and what treatments you're eligible for under your current health plan(s). Traditionally, these requests are made manually, with the whole process taking place over the phone, by email, or maybe even by way of horse and carriage.
Naturally, with the aid of technology, the eligibility and information request process can be automated. And when one considers that there are about two trillion eligibility queries made by hospitals and doctors every year (a single procedure might involve five queries) — one starts to understand the amount of time, money and bandwidth that can be saved by automating those mechanics. In fact, it's now understood to be such a critical need, that the Obama Administration (under its new healthcare policy) has mandated that insurers must begin automating their response to these queries.
Of course, automating and streamlining data exchange in the world of legacy Healthcare IT is easier said than done. Eligible co-founders Katelyn Gleason and Patrice Krakow have embraced the old technologies endemic to Healthcare IT (and the translation burden that comes with it) in order to solve what they believe is a very real (and monumental) problem both for developers and insurers. And, well, really everyone involved in the process (doctors, hospitals, administrators, developers, insurance companies, and, of course, patients).
 Those two trillion queries that are made annually happen across a number of disparate data standards, including those for labs and testing, for insurance info, doctor visit info, pharmaceutical info and so on. That information is critical, but tends to be locked in its own individual silo, and there's not much intercommunication. Aggregating that info becomes exponentially more complicated when you add the fact that there are a huge number of insurance companies providing coverage under an even huger (yep, I said it) array of plans.
Those two trillion queries that are made annually happen across a number of disparate data standards, including those for labs and testing, for insurance info, doctor visit info, pharmaceutical info and so on. That information is critical, but tends to be locked in its own individual silo, and there's not much intercommunication. Aggregating that info becomes exponentially more complicated when you add the fact that there are a huge number of insurance companies providing coverage under an even huger (yep, I said it) array of plans.
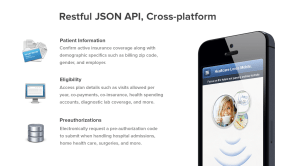
To make it easier on healthcare providers, insurers and everyone in between, Eligible aggregates data from the various insurance providers, normalizing coverage data and patient info from each silo in a stack of REST APIs.
For developers, this means spending a lot less time parsing and for both developers and providers, integration with Eligible's APIs means being able to confirm active insurance coverage and demographics like billing zip codes, gender and employer, as well as being able to get access to plan details, including diagnostic lab coverage, health spending accounts co-payments, and so on. It also makes life easier on hospitals (and developers) by allowing them to electronically request pre-authorization codes for admissions, home health care and surgeries, streamlining the entire care chain, from signing in at the front desk of the hospital to check out.
In the same way Stripe offers developer-friendly technology to simplify the complex and obscure process of integrating payment processing into apps and websites, Eligible wants to build the first modern API that allows developers to easily exchange health data — and make money while doing it. Developers can integrate Eligible to increase both traction and revenue through these eligibility queries, patient information queries, etc.
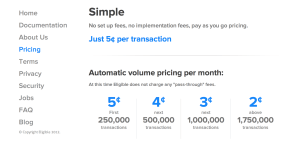 In fact, Gleason tells us that Eligible is already processing 8,000 eligibility transactions per day and, at five cents per transaction, the startup is already producing revenue. The company is already working with more than 100 different providers and healthcare companies and 60 percent of hospitals, and the co-founder says this number is growing fast.
In fact, Gleason tells us that Eligible is already processing 8,000 eligibility transactions per day and, at five cents per transaction, the startup is already producing revenue. The company is already working with more than 100 different providers and healthcare companies and 60 percent of hospitals, and the co-founder says this number is growing fast.
With Obamacare mandating the realtime automation of healthcare eligibility requests and healthcare organizations and startups looking for an easier and more accurate way to access this information for their own apps, Eligible has a real opportunity at turning this early growth into a long-term hockey stick.
Eligible has done the tough leg-work and written the code so that developers and healthcare companies don't have to, and that alone is money in the bank.
The startup has raised $500K in seed capital to date from Y Combinator, Start Fund and a number of other angel investors, including SV Angel's David Lee, Esther Dyson, Anvil Capital's Michael Liou, Accenture Managing Director Anand Swaminathan and Andreessen Horowitz.
After graduating from Y Combinator with the foundation of its healthcare information exchange platform in place, the team joined Rock Health's accelerator this winter, where the team is currently plugging away.
For more on Eligible, check them out at home here.
No hay comentarios:
Publicar un comentario